Our clinical sciences research stream is investigating the causes and impacts of common diseases, and translating those findings into more effective treatments for patients on a local, national and global scale.
Our clinical sciences research stream is investigating the causes and impacts of common diseases, and translating those findings into more effective treatments for patients on a local, national and global scale.
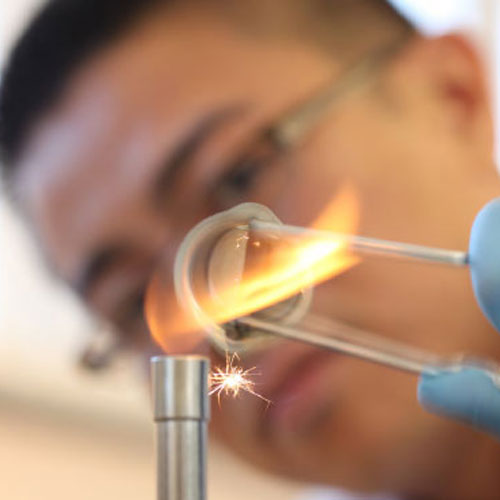
Clinical sciences researchers at the Ingham Institute are working on one of the world’s largest-ever genomic studies to help eradicate the superbug Golden Staph. This antibiotic resistant disease is the cause of major hospital-acquired infections around the world and is an emerging cause of infections in the community. Our scientists are using whole genome sequencing to identify genes, mutations and unique elements that enable these bacteria to thrive in these environments.
Other researchers also are focused on the complications arising from diabetes, the sixth leading cause of death in Australia. South Western Sydney has one of the highest prevalence rates of diabetes in NSW and complications from this disease can significantly impact people’s quality of life. Our scientists are investigating diabetic foot disease, in-patient management, diabetic cardiomyopathy, diabetes in pregnancy, and diabetic retinopathy.
There is also a pressing need for better treatment for people with arthritis and autoimmune disease. Clinical science researchers from our Arthritis Research team are involved in finding and evaluating biomarkers (disease characteristics) and patient-reported outcomes to transform the clinical assessment of patients who have connective tissue diseases.
Strains of methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) are a major cause of healthcare-associated (HA) infections around the world and are concomitant with increased health-care costs, morbidity and mortality; the intractability of such infections is largely due to the capacity of strains to develop resistance to most clinically relevant antibiotics. In this regard, molecular analyses have revealed that widespread multi-resistance has been driven by strong selection pressure and the acquisition of pre-existing determinants, thus highlighting the significant role of mobile genetic elements in the adaptive evolution of these hospital pathogens.
The ARMEGs integrated research program focusses on addressing this global healthcare issue through three main areas of research: molecular epidemiology of pathogen transmission, antibiotic development (i.e., of new/novel compounds) and the evolution of antibiotic resistance, and the role of biofilms as pathogen reservoirs and in various pathologies.
Executive Leadership
Ischaemic heart disease (IHD) is the leading single cause of death in Australia and a significant contributor to the mortality gap between Aboriginal and non-Aboriginal people and to increased morbidity in the ethnically and culturally diverse population of South Western Sydney. Advances in pharmacological and interventional treatments can facilitate enhancements in patient care.
The establishment of ICON, with the commensurate growth in research-led practice, aims to support our district-wide service to respond to the expected ongoing growth of new and more complex cardiovascular cases with new therapies and better care models, ultimately improving mortality rates and long-term patient outcomes. Not only do we expect improved patient outcomes broadly, with specific research investments in Aboriginal and Culturally and Linguistically Diverse (CALD) patient groups, we can create targeted programs which will see mortality rates and outcomes align with our larger patient cohort.
Our academic focus is on innovation and bringing new and existing technologies and procedures to our patients. Key strengths include the groups’ work into imaging research, predominantly in echocardiography, and Acute Coronary Syndrome/ Percutaneous Coronary Intervention research. We have a strong track record of participating in clinical research, both industry supported trials and outcomes research studies as well as local, national, international investigator initiated trials and outcomes research studies. We hope to build on this through our involvement with the Ingham institute. We also focus on collecting reliable data for use in quality assurance projects and ensuring a transformative experience for our patients, particularly those high risk individuals from Aboriginal and Torres Strait Islander backgrounds and the large number of patients from Culturally and Linguistically Diverse populations.
We have a strong culture of teaching and education through our association with the Universities of NSW and Western Sydney. We have had at least 20 successful higher degrees via research (HDR) students and we hope to build on this and provide additional opportunities for post graduate education for postdoctoral Nursing, science and Medical research student candidates.
Our unit actively collaborates with medical oncology, radiation oncology and haematology, and in 2017 the States’ first dedicated cardio-oncology clinic was launched. We have also collaborated with, endocrinology (diabetes), and the Centre for Oral Health Outcomes and Research Translation (COHORT) and oral health services. In recent times we have reached out to the Translational Health Research Institute (THRI) at Western Sydney University and hope to collaborate on research projects and potentially offer more options for postgraduate teaching and education.
We have national collaborations particularly with South Australia (Prof French is a Hon Fellow at the South Australian Health & Medical Research Institute), which includes CIB on the NHMRC funded ACT-2 trial, and internationally via the WNICR group led from the University of Toronto, and national leader of the STREAM-2 trial.
To date we have supported two early career research grants:
Dr James Xu who is studying ways to improve the coronary microcirculation using the index of microcirculatory resistance (IMR) in the setting of non-ST elevation acute coronary syndromes (NSTE-ACS),
Ms Xian Zhou who is studying the nutraceuticals, curcumin and resveratrol and their potential ability to protect the endothelium against oxidative stress using cellular assays and animal models.
We have also employed a research nurse to assess outcomes of patients undergoing cardiovascular procedures.
We are site investigators in a number of large scale clinical trials.
Higher Degree Students:
5
Current Clinical Trials:
– ABBOTT NGDES428 Stent Trial – PI: S Lo
– ACT-2 – PI: J French
– AEGIS ll Study – PI: C Mussap
– Amyloid Study- PI: Louis Wang
– EASY-AS – PI: Dominic Leung
– Heart-FID Study – PI: J French
– HORIZON Trial – Lp(a) –PI: M Leung.
– OASIS 9 – PI: K Asrress
– PIONEER PLUS – PI: M Leung.
– SELECT LIFE – PI: M Leung:
– SELECT trial – PI: M Leung
– STEP HFpEF trial-PI: M Leung
– STREAM-2 – PI: J French
Trials in follow up phase
– ABSORB lV – PI: C Juergens
– DalGeNe –PI: J French
– FAME 3 – PI: K Asrress
Group Co-Leaders
Prof Craig Juergens & Prof John French
The Correlative Microscopy Group was formed in 2013 with the mission to apply correlative microscopy (CLEM) techniques to enhance the study of disease processes in human tissue samples. This emerging technology aims to integrate “form and function” information from multiple microscopy modalities for improved visualisation of disease related changes. This approach covers multiple scales from the organ level to the single molecule.
Our practical aim is to maximise the information obtainable from routine human biopsy and surgical tissue samples and to correlate this information with clinical imaging. The power of CLEM lies in linking clinically diagnosed disease to changes or interactions in single cells. Biomarkers can be labelled and their participation in the disease process tracked. Key proteins forming sites of drug action or drug failure can be identified.
We have recently obtained grants from the Cancer Institute of NSW, NSW Health Pathology, Ingham Institute and UNSW Australia to create a new facility to apply this approach in cancer research.
In June 2016 saw the Correlative Microscopy Facility established with a state-of-the-art electron microscope (FESEM) commissioned. This is the first FESEM in Australia dedicated to cancer biomarker detection in human tissue. Optimised to use the combined strengths of cryogenic cell preservation and nanotechnology, it is one of the most powerful microscopes of its type in the world.
In June 2017 a correlative superresolution laser scanning microscope (SRLSM) will be commissioned to complement the facility’s CLEM workflow.
Group Leader
Associate Professor Murray Killingsworth
The Laboratory of Translational Cutaneous Medicine aims to bridge the gaps between basic science, clinical research and bedside patient care in the field of Dermatology.
Our research group is involved in investigations across the various levels of the translational pipeline in various inflammatory skin diseases including Hidradenitis Suppurativa, Pyoderma Gangrenousm, Psoriasis, Atopic Dermatitis and Vitiligo.
T1: Basic Research into the cellular and molecular alterations seen in inflammatory skin diseases
T2: Proof-of-concept studies of novel therapeutic targets and re-purposing of existing therapeutics in inflammatory skin diseases.
T3: Development and Validation studies of patient-based outcome measures and therapeutic biomarkers in inflammatory skin disease
T4: Population based studies of disease prevalence, therapeutic efficacy, biomarker validation studies and international collaborations in guideline development in various inflammatory skin diseases.
Laboratory head: Dr John W Frew MBBS MMed MS PhD FACD
Research Fellow: Dr Emily Kozera
Post-Graduate Research Student: Dr Akshay Flora
For further information please contact Dr Frew at john.frew@unsw.edu.au
Our aim is to understand the molecular mechanisms regulating liver inflammation, fibrosis, cirrhosis and cancer as well as using transgenic animals to model human liver disease with a view to developing novel therapeutic agents as well as new tools for diagnostic investigations.
The current focus of the research group is to further understand the role of the glycoprotein CD147 (extracellular matrix metalloproteinase inducer; EMMPRIN) in mediating basic and fundamental aspects of tissue inflammatory responses and carcinogenesis. Our group has made the fundamental discovery that CD147 mediates a process of inflammatory cell aggregation, which determines the extent of liver injury. Based on this novel discovery we found that if CD147 is blocked in vivo a marked reduction in liver injury was seen in mouse models of liver disease, which has the potential to lead to new therapeutic agents.
Clinical research undertaken by his group examines the use of probiotics to change the composition of the gut flora, treatment of muscle cramps, the use biomarker predictors of liver injury and nutritional interventions in end stage liver disease.
Immune Tolerance Group leaders Associate Professor Suzanne J Hodgkinson and Professor Bruce M Hall and their team focus on T regulatory cells and how to enhance natural immune regulation mediated by these cells. Immunology Tolerance is a state where the immune system controls by self-regulating processes immune mediate inflammation. These natural processes can prevent rejection of organ and bone marrow grafts as well as prevent or cure autoimmunity. Autoimmune diseases affect up to 10% of the Australian population and include juvenile diabetes, multiple sclerosis, nephritis of the kidney, inflammatory bowel disease and many forms of arthritis.
The key mediator of immune tolerance is a specialized regulatory cell population that is known as CD4+CD25+T regulator cell (Treg). This cell was first described by Professor Hall’s group in Australia and is now studied worldwide. Therapy with this cells to prevent transplant rejection and cure juvenile diabetes is being trialled in the US and Europe.
The regulator cells can also have undesirable effects, preventing the immune system eliminating cancers and chronic infections. New therapies that block their function, can lead to cancer cures.
The group’s work is very different to that done elsewhere. Most studies examine a regulatory cell that inhibits all immune responses, our group studies cells that only suppress the unwanted immune response. We can activate these specific cells in culture and transfer them to prevent rejection or autoimmunity in animal models. The group has identified two pathways of activation of antigen specific Treg based on the novel cytokine receptor expression in rodent models.
We are now focussed on their comprehensive characterization and extending our animal work to humans, specifically how to activate antigen-specific T regulatory cells in culture and in the host. We are also developing methods to monitor antigen specific T regulatory cells in patients. We are focussing on therapy and monitoring for Multiple Sclerosis and organ transplants. Studies are underway looking at these cells in Multiple Sclerosis and the newer therapies.
These studies are world leading and have major therapeutic potential in transplant rejection and autoimmunity. Our cells are over 1000 fold more potent than those being tested overseas and are specific. With adequate funding we could apply these findings to trials in therapy within a few years. Hundreds of thousands of patients world-wide could benefit from such therapy.
Group Leaders
Professor Bruce Hall & Associate Professor Suzanne Hodgkinson
The Immunology team (A/Prof John Quin, Dr Louise Evans and Dr Catherine Toong) are committed to improving the diagnosis and treatment of patients with immune-mediated diseases. The Unit is involved in a randomised controlled trial to investigate the efficacy of new medication in HIV affected patients. Research into the use and improvement of diagnostic tests for autoimmune diseases such as systemic lupus erythematosus (SLE) is continuing. A number of other diagnostic laboratory audits and quality control measures are underway.
The Department of Respiratory Medicine is conducting clinical research in diverse fields including asthma, COPD, bronchiectasis, sleep disorders, tuberculosis and interventional pulmonology. In addition, several of our researchers are engaged in public health and epidemiological research on sleep disorders, tuberculosis, asthma and COPD. Some of the studies we are currently running include:
The Rheumatology Research Group are focused on improving the lives of people with musculoskeletal and autoimmune diseases. The group has embedded research into clinical practice at Liverpool Hospital, with a patient centred approach that records patient reported outcome measures at every visit.
The Rheumatology Research Group offer a variety of sub-speciality clinics that focus on specific groups, including those with psoriatic arthritis, systemic lupus erythematosus and systemic sclerosis, allowing a variety of clinical and laboratory projects. Our collaborations include research into the 3 most common musculoskeletal conditions: osteoarthritis, osteoporosis and back pain.
The group participate in a number of other national and international collaborations including the Asia Pacific Lupus Collaboration, the Australian Lupus Registry and Biobank and the Australian Scleroderma Interest Group. The group offer a number of supervised research projects for undergraduate and postgraduate research students, and includes a clinical trials unit that participates in numerous multicentre studies.
South Western Sydney Stroke and Neurology Group (SWS Strong) is a collaboration of clinicians and researchers from South Western Sydney Local Health District (SWSLHD) and the Ingham Institute for Applied Medical Research. Led by Associate Professor Dennis Cordato, SWS Strong is one group belonging to the Ingham Institute’s expansive Clinical Sciences research stream.
The group focuses their research on stroke and neuroscience, with a number of existing research opportunities for Independent Learning Projects (ILP), Honours, Masters, and Doctor of Philosophy (Ph.D.) students available.
SWSLHD has one of the largest stroke referral centres in NSW, including an active endovascular clot retrieval service. SWS Strong has a special interest in providing excellence in the diagnosis and management of acute stroke patients.
SWS Strong have dedicated clinical trials and research staff tasked with leading the community, driving research, and participating in a number of multicentre international clinical trials.
To learn more about SWS Strong, click here.
Group Leader
Associate Professor Dennis Cordato
The loss of a limb is devastating for those experiencing it. Limb loss is seen commonly as a consequence of severe traumatic injury, cancer ablation, ulceration associated with diabetes, non-diabetes associated wounds, peripheral vascular disease and skin and soft tissue / bone infection. The most common forms of amputation in Australia occur in the lower limb from the effects of vascular disease and or diabetes. Diabetes has increased in south Western Sydney by over 158 per cent since the year 2000. About 13% of the South Western Sydney population have diabetes compared to 8.7% for the state and 7.4% nationally. Over the next 15 years, growth in the district is expected to increase by over 300,000 people. With the continuing upward trend of diabetes prevalence and population growth, there is a strong likelihood that lower and upper extremity complications such as wounds or amputations will also increase. Wounds of the limbs and limb loss are an under-researched area in Australian health care, and often overlooked in terms of public policy. In addition to the direct impact on quality of life, wounds and limb loss impose substantial costs to the health care system and to patients. The Five-year mortality and direct costs of care for people with diabetic foot complications for example are comparable to cancer.
The vision of the Limb preservation and Wound Research Academic Unit is to; become world leaders in the respective fields of limb preservation and wound research through undertaking high-quality sustainable research through nurturing local talent and to translate our research findings into improving the care of people in South Western Sydney (locally) and more widely at a global level. Our vision will help us to reduce avoidable amputations, excel in clinical care, be leaders in limb preservation and wound research and improve the quality of life of people in South Western Sydney.
The Specific research aims and areas of priority over the next five years (2018 -2023) will include:
• Infection of skin, soft tissue and bone
• Wound Repair and regeneration
• Charcot neuroarthropathy
• Development of new or novel therapies and medical devices
• Improving clinical care in Limb preservation / High Risk Foot Services
Neurology & Stroke is one of the Research Centres at Ingham Institute Liverpool. The location next to Liverpool Hospital allows the co-location of research, education and clinical practice.
What we do
We’re a neurology-focused research group specialising in stroke. Our research group in includes a diverse set of individuals and skill sets.
Research Group Impact
We’re currently running several clinical trials across all phases in an effort to improve individuals’ outcomes after a stroke or neurology event.
By searching for new treatments, improving what we currently have, or better assessing patients we’re striving to support people during one of their most difficult times.
Benefit to Community
So far, we’ve led the country in acute stroke research by:
• improving stroke identification pre-hospital
• developing new brain imaging tools to support stroke diagnosis and treatment
• completing world-leading trials that have changed global clinical practice
Group Leaders
Mark Parsons
Major Accomplishments / Awards
• 11 publications
• grants >$1.3m
• Ingham Institute Research Excellence Awards 2022 (Lady Mary Fairfax AC, OBE Distinguished Researcher Award)
To learn more about Mark Parsons and the Sydney Brain Centre, click here.
Group Leader
Mark Parsons
The focus of this multi-disciplinary group is to investigate the use of bedside technology to better phenotype underlying mechanisms of disease and guide personalised treatment in critically ill populations. We have collaborations with Intensive Care colleagues at Bankstown, St George and Hunter Hospitals, NSW, and Oxford University Hospitals UK, as well as with scientists from the Monash and Australian National Universities.
Group Members:
Group Leader
Professor Anders Aneman
To learn more about the Ingham Institute or to book a tour contact us today.